As healthcare providers navigate the complex world of insurance, prior authorization is a critical component of ensuring patients receive the care they need. Molina Healthcare is a leading provider of health insurance in the United States, and their prior authorization lookup tool is an essential resource for healthcare providers. In this article, we’ll explore what the Molina prior authorization lookup tool is, how it works, and why it’s so important.
What is the Molina Prior Authorization Lookup Tool?
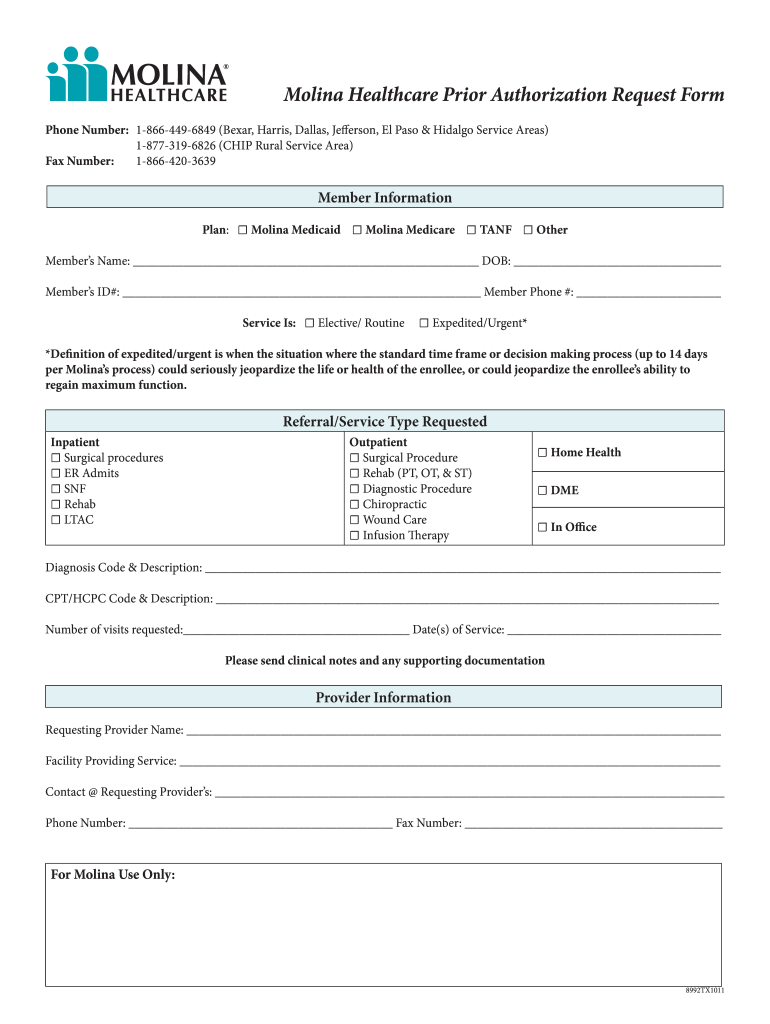
The Molina prior authorization lookup tool is an online resource that allows healthcare providers to quickly and easily check whether a particular service or procedure requires prior authorization from Molina Healthcare. By entering the appropriate CPT code or HCPCS code into the lookup tool, providers can get instant confirmation as to whether prior authorization is required.
How does the Molina Prior Authorization Lookup Tool work?
Using the Molina prior authorization lookup tool is simple and straightforward. First, healthcare providers must have access to the Molina provider portal. Once logged in, they can navigate to the prior authorization lookup tool and enter either a CPT code or HCPCS code. The tool will then display whether prior authorization is required or not. If prior authorization is required, providers can initiate the process through the portal.
Why is the Molina Prior Authorization Lookup Tool important?
Prior authorization can be a time-consuming and frustrating process for healthcare providers. Without a reliable way to determine whether a particular service or procedure requires prior authorization, providers may waste valuable time submitting requests that are ultimately denied. The Molina prior authorization lookup tool streamlines this process by providing instant confirmation as to whether prior authorization is required. This helps providers make more informed decisions about patient care and reduces administrative burdens.
Benefits of Using the Molina Prior Authorization Lookup Tool
There are several benefits to using the Molina prior authorization lookup tool:
1. Saves Time: Providers can quickly determine whether prior authorization is required, saving time and reducing administrative burdens.
2. Improves Efficiency: By streamlining the prior authorization process, providers can focus on delivering high-quality patient care.
3. Reduces Denials: By ensuring that only appropriate services are submitted for prior authorization, providers can reduce the likelihood of denials and improve revenue cycle management.
4. Enhances Patient Care: With the ability to quickly and easily determine whether a service requires prior authorization, providers can make more informed decisions about patient care.
5. Increases Revenue: By reducing denials and improving revenue cycle management, providers can increase their bottom line.
Tips for Using the Molina Prior Authorization Lookup Tool
While the Molina prior authorization lookup tool is an essential resource for healthcare providers, there are a few tips to keep in mind:
1. Check regularly for updates: The codes that require prior authorization may change over time, so it’s important to check regularly for updates.
2. Double-check before submitting requests: While the tool provides accurate information, it’s always a good idea to double-check before submitting a request for prior authorization.
3. Use other resources as needed: While the Molina prior authorization lookup tool is a great resource, it’s not the only one available. Providers should also consult with their billing department or refer to Molina Healthcare’s provider manual when necessary.
Conclusion
The Molina prior authorization lookup tool is an essential resource for healthcare providers navigating the complex world of insurance. By providing instant confirmation as to whether a particular service or procedure requires prior authorization, this tool saves time, improves efficiency, reduces denials, enhances patient care, and increases revenue. As healthcare continues to evolve, tools like the Molina prior authorization lookup tool will become increasingly important in ensuring high-quality care for patients.
References:
Molina Healthcare – Provider Manual (https://www.molinahealthcare.com/providers/oh/manuals/prior-authorization.aspx)
CPT Codes Lookup – Molina Healthcare (https://provider.molinahealthcare.com/Provider/SearchTools/CPTCodesLookup)