In the world of healthcare administration, it’s all about being efficient and streamlined. Medical professionals need to be able to manage their patients’ care in a timely manner, while insurance providers need to ensure that they’re providing coverage only for necessary procedures. That’s where the Molina prior auth tool comes in.
If you’re not already familiar with prior authorization, it’s essentially a process by which an insurance provider reviews a medical request before approving it. This can include anything from medication prescriptions to diagnostic imaging tests and surgical procedures. The goal is to ensure that the requested service is medically necessary and cost-effective.
However, the prior auth process can be incredibly time-consuming and frustrating for both medical professionals and patients alike. That’s where Molina’s prior auth tool comes in – it simplifies the process and makes everything run more smoothly.
So what exactly is the Molina prior auth tool? Let’s dive into some of its key features and benefits.
[h2]What Is the Molina Prior Auth Tool?[/h2]
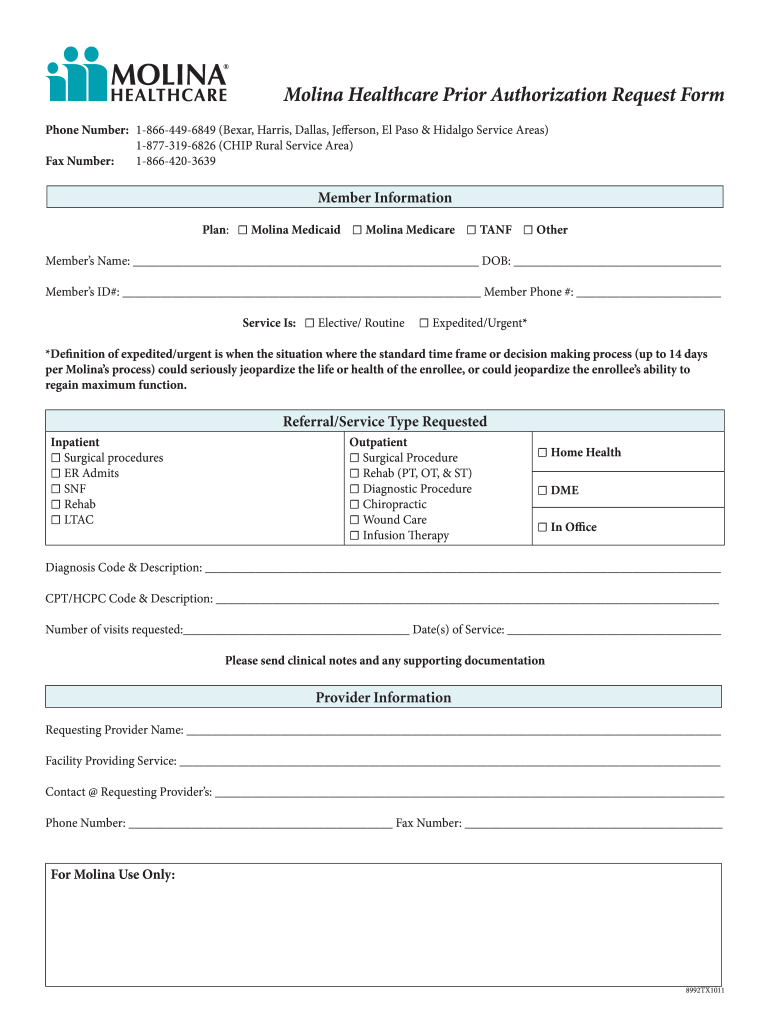
The Molina prior auth tool is essentially an online portal that allows medical professionals to submit prior authorization requests quickly and easily. It takes much of the guesswork out of the process, providing clear guidelines on what information is required for each type of request.
[h2]How Does It Work?[/h2]
Medical professionals simply log in to the Molina prior auth tool using their credentials, then select the type of request they want to submit (e.g., medication or procedure). From there, they’ll be prompted to fill out all of the necessary information, such as patient details, diagnosis codes, and treatment plans.
Once the request has been submitted, it will be reviewed by Molina’s team of experts. They’ll determine whether or not the requested service is medically necessary and cost-effective based on your submission, as well as any additional information they may need.
[h2]What Are the Benefits of Using the Molina Prior Auth Tool?[/h2]
There are a number of benefits to using the Molina prior auth tool, both for medical professionals and patients. Let’s take a look at some of them.
[1] Faster Turnaround Times
One of the biggest advantages of using the Molina prior auth tool is that it can significantly speed up the prior authorization process. Because everything is done online, there’s no need to wait for faxes or phone calls – requests can be submitted and reviewed in real-time. This means faster turnaround times for medical professionals and patients alike.
[2] Clear Guidelines and Requirements
Another key benefit of the Molina prior auth tool is that it provides clear guidelines and requirements for each type of request. This takes much of the guesswork out of the process, helping to ensure that requests are submitted correctly and completely. It also reduces the likelihood of requests being denied due to missing or incorrect information.
[3] Reduced Administrative Burden
Prior authorizations can be incredibly time-consuming and frustrating for medical professionals, taking them away from patient care and adding to their administrative burden. By streamlining the process with an online portal like Molina’s, much of this burden can be lifted. Medical professionals can spend less time on paperwork and more time providing care to their patients.
[4] Improved Patient Outcomes
Ultimately, the goal of prior authorization is to ensure that patients receive medically necessary and cost-effective care. The Molina prior auth tool helps to achieve this by making it easier for medical professionals to submit requests quickly and accurately. This means that patients can receive the care they need more quickly, leading to improved outcomes overall.
[h2]Conclusion[/h2]
In summary, if you’re looking to simplify your healthcare administration process, consider using the Molina prior auth tool. It’s an easy-to-use online portal that can help you submit prior authorization requests quickly and accurately, reducing administrative burden and improving patient outcomes. Give it a try today and see the difference for yourself.
References:
https://www.molinahealthcare.com/providers/medicaid/prior-auth.aspx
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/MedicareProviderSupEnroll/Prior-Authorization-Process.html